Neuromonitoring Burkhard Simma Traunseeklausur Gmunden
←
→
Transkription von Seiteninhalten
Wenn Ihr Browser die Seite nicht korrekt rendert, bitte, lesen Sie den Inhalt der Seite unten
Monitoring ist die Beobachtung einer Erkrankung, eines Symptoms u/o eines (oder mehrerer) medizinischen Parameters über die Zeit …durch kontinuierlich gemessene Parameter durch einen Monitor oder Vitalzeichen oder durch wiederholt durchgeführte Tests (z.B. Glucosemonitoring)
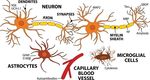
Neuromonitoring Der kontinuierlich gemessene Hirndruck ist die essentielle Modalität….. Nach Jahren der enthusiastischen Anwendung/Forschung des Hirn-Monitorings (z.B. Gewebssauerstoff, Mikrodialyse, CBF, Transkranieller Doppler, V. jugularis Sättigung, NIRS) bleibt die Hirndruckmessung als robuste und einzige nur moderat invasive Modalität übrig, die auch von den meisten PICU realistischerweise durchgeführt werden kann Tasker RC in Fuhrman and Zimmerman (eds). Pediatric Critical Care 5th ed 2017
NEURO - Monitoring
Kontinuierlich vs. intermittierend
Nicht-invasiv vs. invasiv
Validiert vs. experimentell
Klinische Untersuchung
Physiologisches Monitoring
Labor Analysen (Biomarker)
BildgebungMonitoring und Pädiatrische Trauma Zentren
Basel
Bern
Genf
Lausanne
Luzern
St. Gallen
Zürich
Level I Pädiatrisches Trauma Zentrum: Injury Severity Score >(12)16
(Hochspezialisierte Medizin, HSM; CH)Summe der Quadrate der drei hauptsächlich betroffenen Organe Level I Pädiatrisches Trauma Zentrum: Injury Severity Score >(12)16 (Hochspezialisierte Medizin, HSM; CH)
Klinische Untersuchung
Glasgow Coma Scale (GCS) Score und Mortalität
Bei Kindern jünger als 5a wurde eine ähnliche Relation zwischen GCS und Mortalität beobachet
Murphy S, J Neurotrauma 2017Schweres Schädel Hirn Trauma
Erst-Linie Interventionen
HOB 30°
Sedierung und Analgesie
Anlage ICP Monitor –
CSF Drainage
Neuromuskuläre Blockade
Hyperosmolare Therapie
Normoventilation
SpO2 >92%
Adelson PD. PCCM 2003;4:565; Carcillo JA. CCM 2006;34:S183ICP Monitoring
ICP Messung ermöglicht
Kalkulation des zerebralen Perfusionsdruckes (als therapeutische Zielgröße)
Analyse der ICP Kurven
Ableitung der zerebrovaskulären Druck Reaktivität und der
Kompensatorischen Reserve
Nulllinie von ICP und arteriellem Druck auf gleicher Höhe:
Tragus des OhresICP Kurvenanalyse – zerebrovaskuläre Druck Reaktivität
Pressure reactivity (PRx) Index:
Kalkulation des Korrelationskoeffizienten aus >40 Datenpunkten
von arteriellem Druck (ABP) und ICP
(Antwort des ICP auf spontane Änderungen des ABP)
PRx: negativ oder nahe Null
jeder Anstieg des ABP führt zu einer inversen Änderung
des ICP: d.h. CBV normal
Positiver Index: nicht-reaktives Gefäßbett
Tasker RC in Fuhrman & Zimmerman (eds). Pediatric Critical Care 5th ed 2017ICP Kurvenanalyse
Analyse der Frequenz der ICP Kurve
Frequenz ist ähnlich der Herz- und Atemfrequenz und es gibt „slow waves"
(3-0.3 Zyklen pro Minute)"
Amplitude der Puls Welle
(fundamental component)
korreliert mit zerebralem Blutvolumen
Tasker RC in Fuhrman & Zimmerman (eds). Pediatric Critical Care 5th ed 2017ICP Kurvenanalyse - Kompensatorische Reserve
RAP index: Korrelationskoeffizienten (R) zwischen Pulse Amplitude (A) und mittlerem ICP (P)
Index nahe Null: fehlende Synchronisation: d.h. Änderungen/Steigerung des Volumens führt nicht zu
einem höheren ICP = good pressure-volume reserve.
Index steigt +1: Änderung des Volumens erhöht ICP: kompensatorische Reserve ist gering
Tasker RC in Fuhrman & Zimmerman (eds). Pediatric Critical Care 5th ed 2017ICP Kurvenanalyse - Kompensatorische Reserve
RAP index: Korrelation Koeffizient (R) zwischen Pulse Amplitude (A) und mittleren ICP) (P)
Index nahe Null: fehlende Synchronization: d.h. Änderungen/Steigerung des Volumes führt nicht zu
einem höheren ICP = good pressure-volume reserve.
Index steigt
RAP +1:und
Änderung des Reactivity
Pressure Volumen erhöht
(PRx)ICP: kompensatorische Reserve ist gering
Index
„…are predictive of poor outcome in adults
may be useful in definition of optimal targets for CPP…“
Eine Studie bei Kindern/Jugendlichen n=21
Tasker RC in Fuhrman & Zimmerman (eds). Pediatric Critical Care 5th ed 2017Multizentrisch, n=324, >13a
ICP basierendes Protokoll vs. bildgestütztes und klinisches Protokoll
Endpunkte: Zeit Überleben, eingeschränktes Bewusstsein; funktioneller und kognitiver Status nach 6 Monaten
ICP Imaging-clinical
group
__________________________________________________________________________________________ _
6 mo neuro status (points) 56 53
6 mo mortality (%) 39 41
ICU stay (days) 12 9
Craniectomy (%) 28 30
Brain-specific treatments (days) 4.8 3.4 .002
Hypertonic saline (%) 58 72 .008
any serious event (%) 45 46
BEST-TRIP: Benchmark Evidence from South American Trials: Treatment of Intracranial PressureNational Trauma Data Bank Pediatric Health Information System database n>3000 Kinder/Jugendliche Primäre Endpunkte: Krankenhaus Mortalität, Entlassung in Hospiz, oder neue Tracheostomie u/o Gastrostomie [GT]
Transcranieller Doppler (TCD)
Messung der zerebralen Blutflussgeschwindigkeit
Grenze: >100cm/sec zeigt Vasospasmus oder Hyperämie an
Lindegaard Ratio: untersuchte A. cerebri media und ipsilaterale A. carot. int.
>3 VasospamusMicrodialyse Wird platziert im rechten (nicht dominanten) Frontallappen oder ipsilateral der Läsion für Monitoring des Gewebes unter Risiko und zur Steuerung der Therapie multiple Katheter sind eine Option, 100 KDa Membran stündliche Messung von Glukose, Laktat, Pyruvat, Glycerol und Glutamaten Wird sehr früh bei sekundären Schädigungen auffällig
Microdialyse Glukose:
Somatosensory evoked potentials (SSEP) 134 adults, after cardiac arrest and hypothermia Clinical examination (p
Multimodales Neuromonitoring (MMM)
Erwachsene Pat (n=27) mit niederem regionalem zerebralem Blutfluss (=Hypoperfusion im CT) vs.
normalem Fluss
- erhöhter ICP 30 vs 13%
- PbtO2NEURO - Monitoring
Kontinuierlich vs. intermittierend
Nicht-invasiv vs. invasiv
Validiert vs. experimentell
Klinische Untersuchung
Physiologisches Monitoring
Labor Analysen (Biomarker)
BildgebungHypertones Kochsalz
Ziel: Serum Sodium 155 mmol/L
CCM 1998Hypertones Kochsalz
Richtlinie für schweres SHT – Hypertones Kochsalz (HS)
3 Studien bei 121 pädiatrischen Patienten aus 2 Zentren
„Hypertonic saline should be considered for the
- acute treatment of elevated intracranial pressure
(evidence class II) and
- use as a continuous infusion at the ICU (class III)”
Effektive akute Dosis : Bolus 3% HS: 3 ml/kg
kontinuierlich 3% HS: 0.1-1.0 ml/kg/h
Ziel: Serum OsmolalitätBiomarker Harel A, 2016
Biomarker in Trauma und Kreislaufstillstand Prout AJ, 2017
Harel A, 2016
PCCM 2009
NEURO - Monitoring
Kontinuierlich vs. intermittierend
Nicht-invasiv vs. invasiv
Validiert vs. experimentell
Klinische Untersuchung
Physiologisches Monitoring
Labor Analysen (Biomarker)
BildgebungNeuro - Bildgebung
ADC: Apparent Diffusion Coefficient
(Diffusionskoeffizient)
diffusion of water molecules to generate
contrast in MR images
hohe ADC: vasogenes Ödem
niedere ADC: zytotoxisches Ödem, Ischämie
Frontiers Neurol. 2015Neuro - Bildgebung ADC: Normalwerte und Prognose Grenzwert: 650–700 × 10−6 mm2/sec Anteil des Gehirnvolumens mit einer ADC
relatives Volumen von Voxel (y-achse) mit einem ADC Wert unter dem definierten Grenzwert (x-Achse) Rescuscitation 2016;100:18-24
ADC and NSE in cardiac arrest ©Scholefield B
Vielen Dank
Monitoring and Cognition Your focus determines your reality You see only what you know Cognition depends on how you feel
Monitoring and Trauma Room
©M. Nance. CHOP, 2016Monitoring and Trauma Room
?
©M. Nance. CHOP, 2016Monitoring and Trauma Room
?
©M. Nance. CHOP, 2016Monitoring and Trauma Room
©M. Nance. CHOP, 2016Monitoring and Trauma Room
Your focus determines your reality -
©M. Nance. CHOP, 2016Monitoring and Cognition Your focus determines your reality You see only what you know Cognition depends on how you feel
Diagnosis?
Diagnosis? Do you notice anything unusual about this lung scan?
Harvard researchers found that 83% of radiologists didn‘t notice the gorilla in the top right portion of this image.
Monitoring and Cognition Your focus determines your reality You see only what you know Cognition depends on how you feel
Why neuro-monitoring, even multi modality monitoring?
• Clinical exmination
• Understand pathophysiology
• Improve protocols and patient management
• Prognostication
• Monitoring and cognitionCerebral Perfusion Pressure - Autoregulation
Perfusion-pressure - based
…MAP limits of autoregulation shift to the left
…may be lost in critically ill children infants
adults
…difference between the actual cerebral perfusion
pressure and the lower limit of autoregulation
auto regulatory reserve
Shoykhet M in Fuhrman & Zimmerman (eds). Peciatric Critical Care 5th ed 2017Cerebral Perfusion Pressure - Autoregulation
Perfusion-pressure - based
…MAP limits of autoregulation shift to the left
…may be lost in critically ill children
…difference between the actual CPP
and the lower limit of autoregulation
auto regulatory reserve
LDF…Laser Doppler FlowmetryCerebral Perfusion Pressure - Autoregulatory reservere
Auto regulatory reserve
may change over time
Assessment
• elevation of blood pressure by medication
• transient hyperemia after carotid compression
• to monitor the natural variation of blood pressure
Tasker RS in Fuhrman & Zimmerman (eds). Pediatric Critical Care 5th ed 2017Cerebral Blood Flow
... gray matter CBF reaches a plateau at 4 yrs of age
…white matter CBF also increases but not as significantly
32 weeks of gestation: 14 mL/100 g/min
Term: 20
4-12yrs 90-100
Adult 50-60
Shoykhet M in Fuhrman & Zimmerman (eds). Peciatric Critical Care 5th ed 2017Cerebral Blood Flow - autoregulation
CBF depends on
pH-based
…CBF changes by 1 (-4)% per for every
1 mmHg change in PaCO2 in the range
of 20-100mmHg
… Hypercapnia causes cerebral vasodilatation,
increases CBF and ICP
Shoykhet M in Fuhrman & Zimmerman (eds). Peciatric Critical Care 5th ed 2017Cerebral Blood Flow - autoregulation CBF depends on Oxygen-based …CBF is constant when PaO2 is >60mmHg (pink curve) …CBF increases (exponentially) when PaO2
References Allen B eta al. Pediatr Crit Care Med 2014;15:62-70 Gupta AK, Hutchinson PJ, Fryer T, Al-Rawi PG, Parry DA, Minhas PS, Kett-White R, Kirkpatrick PJ, Mathews JC, Downey S, Aigbirhio F, Clark J, Pickard JD, Menon DK. Measurement of brain tissue oxygenation performed using positron emission tomography scanning to validate a novel monitoring method. J Neurosurg. 2002 Feb;96(2):263-8. Ushewokunze S, Sgouros S. Brain tissue oxygenation changes in children during the first 24 h following head injury. Childs Nerv Syst. 2009 Mar;25(3):341-5 Bouzat P, Marques-Vidal P, Zerlauth J-B, et al. Accuracy of brain multimodal monitoring to detect cerebral hypoperfusion after traumatic brain injury. Crit Care Med 2015;43:445–52. Oddo M, Levine JM, Mackenzie L, et al. Brain hypoxia is associated with short- term outcome after severe traumatic brain injury independently of intracranial hypertension and low cerebral perfusion pressure. Neurosurgery 2011;69:1037–45 Kosty JA, Leroux PD, Levine J, et al. Brief report: a comparison of clinical and research practices in measuring cerebral perfusion pressure: a literature review and practitioner survey. Anesth Analg 2013;117:694–8.
CSF volume: adult 150 mL (50% intracranial, 50% intraspinal)
Newborn 50 mL
production through all age groups:
0.15-0.3 mL/min
9-18 mL/h=216-432 mL/dClinical examination Glasgow Coma Scale (GCS) is a neurological scale which aims to give a reliable and objective way of recording the conscious state of a person for initial as well as subsequent assessment. The initial indication for use of the GCS was serial assessments of patients with traumatic brain injury[1] and coma for at least 6 hours in the neurosurgical ICU setting, GCS was initially used to assess level of consciousness after head injury, and the scale is now used by first responders, EMS, nurses and doctors as being applicable to all acute medical and trauma patients. In hospitals it is also used in monitoring chronic patients in intensive care. GCS is used as part of several ICU scoring systems, including APACHE II, SAPS II, and SOFA, to assess the status of the central nervous system, as it was designed for. though it is commonly used throughout hospital departments Individual elements as well as the sum of the score are important. Hence, the score is expressed in the form "GCS 9 = E2 V4 M3 at 07:35“ false positiv: focal neurological signs The GCS has come under pressure from some researchers who take issue with the scale's poor inter-rater reliability and lack of prognostic utility (Green S. M. (2011). "Cheerio, Laddie! Bidding Farewell to the Glasgow Coma Scale". Annals of Emergency Medicine. 58 (5): 427–430). there is no agreed-upon alternative, newer scores such as the Simplified motor scale and FOUR score have also been developed as improvements to the GCS.[8] Although the inter-rater reliability of these newer scores has been slightly higher than that of the GCS, they have not gained consensus as replacements. Available, simple, quick, non-inavsive, validated
Clinical examination FOUR (Full Outline of UnResponsiveness) score Eye and motor responses, brainstem reflexes, and breathing pattern 17-point (0-16) scale Non- or slightly sedated pts More complete in assessment of brainstem function Better inter-rater reliability, sensitivity and PPV than GCS Experience is limited No pediatric studies (as GCS)
ICP Monitoring – w/o invasive transducers Transcranial Doppler technique Optic nerve sonography (sheath diameter) Normal:
ICP monitoring
1. We recommend the continuous assessment and monitoring of ICP and CPP
including waveform quality using a structured protocol to ensure accuracy and
reliability. Instantaneous ICP values should be interpreted in the context of
monitoring trends, CPP, and clinical evaluation.
(Strong recommendation, high quality of evidence.)
2. ICP and CPP monitoring are recommended as a part of protocol-driven care in
patients who are at risk of elevated intracranial pressure based on clinical and/or
imaging features.
(Strong recommendation, moderate quality of evidence.)
3. We recommend that ICP and CPP monitoring be used to guide medical and
surgical interventions and to detect life-threatening imminent herniation; however,
the threshold value of ICP is uncertain on the basis of the literature.
(Strong recommendation, high quality of evidence.)
4. Several studies confirm that brain hypoxia/ischemia can occur when ICP and CPP
are within established thresholds for normality.
5. Elevated ICP values can arise from both increased CBF (hyperemia) and reduced
CBF secondary to cerebral edema, highlighting the nonspecific nature of ICP
readings. (oder aufgeteilt auf zwei Folien, wie nachstehend) Le Roux P. ICM 2014ICP monitoring
1. We recommend the continuous assessment
and monitoring of ICP and CPP including
waveform quality using a structured protocol to
ensure accuracy and reliability. Instantaneous
ICP values should be interpreted in the context
of monitoring trends, CPP, and clinical
evaluation. (Strong recommendation, high
quality of evidence.)
2. ICP and CPP monitoring are recommended as
a part of protocol-driven care in patients who
are at risk of elevated intracranial pressure
Le Roux P. ICM 2014ICP monitoring
3. We recommend that ICP and CPP monitoring
be used to guide medical and surgical
interventions and to detect life-threatening
imminent herniation; however, the threshold
value of ICP is uncertain on the basis of the
literature.
(Strong recommendation, high quality of
evidence.)
4. Several studies confirm that brain hypoxia/ischemia can occur when ICP
and CPP are within established thresholds for normality.
5. Elevated ICP values can arise from both increased CBF (hyperemia)
Le Roux P.and
ICM 2014ICP monitoring
Use of ICP monitoring may be considered
• both, parenchymal ICP monitors and external ventricular
catheters (EVD) provide reliable and accurate data
• association of intracranial hypertension and poor neurologic
outcome
• improved outcomes associated with successful ICP - lowering
therapies
• ICP per se does not provide a useful prognostic marker of
functional outcome
Kochanek PM. PCCM 2012; Le Roux P. ICM 2014The recommendations for an optimal CPP have changed over time and may in
part be associated with the variability in how mean arterial pressure (MAP) is
measured to determine CPP.
Zero reference points for both MAP and ICP should be the same, that is, at the
level of the brain using the tragus of the ear as the external landmark especially in
tall patients
A recent narrative review was unable to determine how MAP was measured in the
calculation of CPP in 50% of 32 widely cited studies of CPP-guided management
Kosty JA. Anesth Analg 2013;117:694-8CPP autoregulation
By ICP (as a surrogate)
transcranial Doppler
near-infrared spectroscopy
No good comparative studies
Thresholds may vary with age and sex (and time)
E.g. pts with preserved autoregulation may benefit from higher blood pressures
N.B. autoregulation is vulnerable in rewarming
Le Roux P. ICM 2014CPP autoregulation
May be useful in broad targeting of cerebral perfusion management goals and
prognostication in acute brain injury.
(Weak recommendation, moderate quality of evidence)
Continuous bedside monitoring is now feasible, and we suggest that should be
considered as a part of MMM. Measurement of pressure reactivity has been
commonly used for this purpose, but many different approaches may be equally
valid.
(Weak recommendation, moderate quality of evidence)
Le Roux P. ICM 2014Transcranial Doppler Pulsatility index ARI = %Δ eCVR/%Δ MAP (ARI = autoregulation index eCVR = estimated cerebrovascular resistance MAP = mean arterial pressure) ≥ 0.4 is normal
Somatosensory evoked potentials (SSEP)
Somatosensory evoked potentials (SSEP) Outcome n=109, SSEP3 in 93% abnormal, but present SSEP: GOS>3 in 63% negative SSEP: GOS
BEST-TRIP: Benchmark Evidence from South American Trials: Treatment of Intracranial Pressure
Microdialysis - adults
We recommend microdialysis in patients with or at risk of cerebral ischemia,
hypoxia, energy failure, and glucose deprivation.
(Strong recommendation, low quality of evidence.)
We recommend that cerebral microdialysis only be used in combination with
clinical indicators and other monitoring modalities for prognostication
(Strong recommendation, low quality of evidence.)
We suggest the use of cerebral microdialysis to assist titration of medical
therapies such as systemic glucose control and the treatment of delayed
cerebral ischemia.
(Weak recommendation, moderate quality of evidence.)
Le Roux P et al. Int Care Med 2014Seizures – monitoring clinical signs & symptoms
Wainwright MS in Fuhrman & Zimmerman (eds). Pediatric Critical Care 5th ed 2017Multimodality neuromonitoring is the
simultaneous measurement of
several variables which allows an
individually tailored approach to the
management of patients with TBI.
Treatment decisions are guided by
monitored changes in
pathophysiologic variables rather
than generic one-size-fits-all
treatment target.
The aim of monitoring is to guide therapy and assist clinicians in decision making
Martinez R 2016ICP monitoring – invasive transducers
ICP monitor only in 60% of patients with severe TBI (GCS≤8)
these hospitals have a lower mortality and disability but have
longer PICU and hospital stay, more ventilator days
⇒ entry criteria for ICP monitor use is not sensitive
Elevated ICP only in 50% of those who had an ICP monitor
only in traumatic axonal injured pts
GCS≤8 predicts ICP>20mmHg
Sens. 80%, Spec. 55%; PPV 68%, NPV 77%
„Any abnormality in CT“ predicts ICP>20mmHg
Sens. 90%, Spec. 94%; PPV 60%, NPV 80%Hemodynamic monitoring
1. We recommend the use of electrocardiography and invasive monitoring of
arterial blood pressure in all unstable or at-risk patients in the ICU.
(Strong Recommendation, moderate quality of evidence.)
2. We recommend that hemodynamic monitoring be used to establish goals that
take into account cerebral blood flow (CBF) and oxygenation.
(Strong recommendation, moderate quality of evidence.)
3. We recommend the use of additional hemodynamic monitoring (e.g.,
intravascular volume assessment, echocardiography, cardiac output
monitors) in selected patients with hemodynamic instability.
(Strong recommendation, moderate quality of evidence.)
4. We suggest that the choice of technique for assessing pre-, after-load,
cardiac output, and global systemic perfusion should be guided by specific
evidence and local expertise.
(Weak recommendation, moderate quality of evidence.)
Le Roux P. ICM 2014Clinical examination
We recommend that assessments with either the GCS (combined with assessment of pupils) or
the FOUR score be routinely performed in comatose adult patients with acute brain injury
(Strong recommendation, low quality of evidence.)
Le Roux P. ICM 2014ICP Wave analysis – compensatory reserve
RAP index: correlation coefficient (R) between pulse amplitude (A) of the
fundamental component (A) and mean (ICP) (P)
Tasker RS in Fuhrman & Zimmerman (eds). Pediatric Critical Care 5th ed 2017Multimodality Neuromonitoring
The challenge is to integrate all data and to avoid misinterpretation: when and how to
treat
It is difficult to demonstrate that any single monitor or combination of monitors has a
positive effect on outcome, because outcome is influenced by the therapeutic plan
driven by monitoring, not by monitoring itself
(1) trends in physiological changes (2) auto regulation (3) optimum CPP (4)
patient-specific thresholds
In the end, MMM is an extension of the clinical examination and cognitive skill of the
clinician, and is only as good or as useful as the clinical team who is using the
monitor and available therapeutic options.
Le Roux P et al. Int Care Med 2014Transcranial Doppler (TCD) Application in adult medicine Static Test of autoregulation blood flow velocity changes during changes of arterial blood pressure by vasopressor infusion Static rate of auto regulation (SoR): percentage increase in vascular resistance divided percentage rise of blood pressure: SoR 100% intact auto regulation; SoR 0% no autoregulation TCD reactivity to changes of PaCO2 cerebral vessels react to changes in PaCO2 when auto regulation is impaired CO22 reactivity correlates with outcome and high PaCO2 elevates ICP Dynamic test of autoregulation index which describes how quickly cerebral vessels react to a sudden fall of ABP
Transcranial Doppler (TCD) Application in adult medicine Static Test of autoregulation blood flow velocity changes during changes of arterial blood pressure by vasopressor infusion Static rate of auto regulation (SoR): percentage increase in vascular resistance divided percentage rise of blood pressure: SoR 100% intact auto regulation; SoR 0% no autoregulation TCD reactivity to changes of PaCO2 cerebral vessels react to changes in PaCO2 when auto regulation is impaired high PaCO2 elevates ICP; CO22 reactivity correlates with outcome Dynamic test of autoregulation index which describes how quickly cerebral vessels react to a sudden fall of ABP
ICP Wave analysis – compensatory reserve
RAP index: correlation coefficient (R) between pulse amplitude (A) of the
fundamental component (A) and mean (ICP) (P)
Tasker RS in Fuhrman & Zimmerman (eds). Pediatric Critical Care 5th ed 2017Cerebral Perfusion Pressure (CPP)
CPP = MAP – ICP
• >(40) 45-50 mmHg infants
• >60 (-65) mmHg children/adolescents
• „Hypertonic resuscitation“
• Vasopressors
Perfusion ≠ Pressure: Flow = ∆P x ∏ x R4/8nl
(Rule of Hagen Poiseuille)
Child Nerv Syst 2004; Crit Care Med 2003NEURO-Monitoring
besteht aus einer Kombination aus klinischer Untersuchung, intrakranieller Druckmessung und Bildgebung
Techniken: Zerebraler Blut Fluss
ICP
CPP
Transcranielle Doppler Sonographie ( TCD); Duplex Sonographie
Thermale Diffusion Flowmetrie (TD)
Zerebrale Oxygenation
V. jugularis Sättigung (SjvO2)
Sauerstoffpartialdruck im Gehirnparenychm(PbtO2)
Zerebral Stoffwechsel
Microdialyse
Globale zerebrale Funktion
EEG
BiomarkerSauerstoffpartialdruck im Gehirn (PbtO2)
Normal: 25-30 mmHg
Grenzwert: 10 (20) mmHg
Niederer PbtO2 kann mit erhöhtem ICP aber nicht mit Prognose korrelieren
ABER er ändert sich auf Interventions
kann Hypoperfusion Areale identifizieren
und gibt zu ICP zusätzliche Informationen
Gupta AK. J Neurosurg 2002; Ushewokunze S. Childs Nerv Syst 2009Brain parenchymal oxygen tension (PbtO2)
Report on 5 children
Gupta AK. J Neurosurg 2002; Ushewokunze S. Childs Nerv Syst 2009Brain parenchymal oxygen tension (PbtO2)
Normal: 25-30 mmHg
Threshold: 10 (20) mmHg
No correlation between the oxygen tension in PET and PbtO2
Low PbtO2 may correlate with elevated ICP and but not with outcome
BUT it changes due to interventions
can identify cerebral hypoperfusion more
reliably than ICP monitoring alone
Gupta AK. J Neurosurg 2002; Ushewokunze S. Childs Nerv Syst 2009NSE und Outcome nach Kreislaufstillstand bei Erwachsenen
Sie können auch lesen